Advanced Laser Therapy:
Unlocking Healing Potential

In recent years, laser therapy has emerged as a powerful, non-invasive treatment option across various medical fields. While its journey to mainstream acceptance, particularly in the United States, has faced historical challenges, a growing body of robust clinical evidence and practical success stories are now solidifying its role as a valuable therapeutic modality.
Historically, the field encountered obstacles from exaggerated claims, a proliferation of thinly veiled marketing disguised as research, and studies hampered by a lack of understanding of critical laser specifications (like power density, irradiance, and fluence) or the use of inadequate equipment. Poorly designed clinical protocols also contributed to skepticism, leading to inconsistent outcomes and a tarnished reputation.
However, the landscape has changed. Today, with advanced technology and a deeper understanding of photobiomodulation, laser therapy is demonstrating consistent and remarkable results, prompting a crucial question: Are we overlooking a truly valuable treatment that could significantly improve patient outcomes?
At OmniLase®, we believe in the proven science and practical benefits of therapeutic lasers. Let’s explore the transformative potential of laser therapy in key clinical areas.
Accelerated Wound Healing: A Proven Advantage
The positive impact of laser therapy on wound healing is one of its most compelling and well-established benefits. Quantitative data from controlled studies show:
- Increased Tensile Strength: Laser treatment enhances the strength of scar tissue, a significant factor in long-term wound integrity.
- Improved Scar Appearance: Especially vital in fields like plastic surgery, laser therapy contributes to a more aesthetically pleasing postoperative scar.
Laser therapy actively supports all three phases of wound healing: inflammation, proliferation, and remodeling. The specific physiological responses are influenced by the laser’s wavelength:
- Pulsed Dye Lasers: Significantly reduce pruritus (itching) during healing and may decrease scar thickness.
- Red Lasers: Stimulate cellular activity, leading to enhanced tissue repair and robust wound epithelialization.
- Violet Lasers: Offer anti-microbial light, contributing to wound sanitation, particularly important in contaminated or complex wounds.
While real-world wounds are often irregular and contaminated—making strictly “purist” scientific controls challenging—clinical practice has consistently shown laser therapy’s effectiveness in promoting the healing of complex cases, such as neuropathic skin ulcers in diabetic patients, where traditional approaches often fall short.
Non-Opioid Pain Management: A Crucial Alternative
Chronic pain affects over 30% of the U.S. population, leading to a profound public health challenge exacerbated by the opioid crisis. Laser therapy emerges as a powerful, non-invasive alternative that has earned FDA approval for various indications, including:
- Relief of muscle and joint pain
- Relaxation of muscles and spasms
- Temporary increase in local blood circulation
- Alleviation of pain and stiffness associated with arthritis
Despite substantial evidence, laser therapy’s full integration into mainstream pain management has been slow, partly due to past inconsistencies. These inconsistencies can often be attributed to a lack of standardized treatment protocols, the use of suboptimal equipment, and an incomplete understanding of pain’s complex etiology.
Understanding Pain and Laser Interaction: Pain is highly subjective and manifests in various forms:
- Nociceptive Pain: Caused by tissue injury (acute or chronic).
- Neuropathic Pain: Caused by nerve damage (predominantly chronic).
- Idiopathic Pain: Of unknown origin (psychological or physiological).
Expecting laser therapy to be a universal panacea for all pain types would be simplistic. However, its effectiveness in specific indications is undeniable. While the exact mechanism of pain suppression by laser therapy is still under investigation, several compelling hypotheses exist:
- Direct Neural Interaction: Light may directly affect neurons, potentially inhibiting axonal transport and altering nerve impulse conduction, leading to rapid pain reduction (observed in acute cases within 30-60 seconds).
- Endorphin Production: Laser therapy might stimulate the release of endorphins, the body’s natural pain-relieving compounds.
- Inflammatory Mediator Suppression: It may prevent the release of prostaglandins and other inflammatory mediators, thereby reducing pain perception.
The ongoing research into these mechanisms continues to refine our understanding, but the immediate practical benefit of laser therapy for pain management should not be delayed by the pursuit of a singular, definitive model. Optimal treatment parameters (wavelength, power, dose, regimen) are best established through ongoing clinical experience and refined protocols.
Mastering Inflammation: A Gentle Yet Potent Approach
Conventional treatment for many inflammatory diseases often relies on immunosuppressive pharmaceuticals, which can carry significant side effects. Laser therapy offers a distinct, non-invasive approach with minimal adverse effects, demonstrating a proven ability to modulate the immune system, especially at the cellular and tissue levels. This positions it as an appealing therapeutic option for a wide array of inflammatory conditions.
Despite promising aspects, some studies have presented conflicting results, primarily due to past inconsistencies in treatment protocols, underscoring the need for precise, standardized methods—a hallmark of OmniLase® technology.
The beneficial effects of laser therapy are rooted in two primary mechanisms:
- Photobiomodulation (Primary Effect): This involves the absorption of infrared light by cytochrome c oxidase, a mitochondrial protein. This absorption accelerates cellular oxygen and metabolite exchange, leading to increased ATP production. ATP serves as the vital energy source for cellular activities, driving faster recovery, enhanced healing, and significant reduction of edema in the treated area.
- Temperature Increase Effect (High-Intensity Lasers): High-intensity laser therapy results in light absorption by water and fat, causing a therapeutic temperature elevation in the tissue. This controlled warmth induces vasodilation, significantly enhancing blood perfusion. The increased blood flow delivers more oxygen and nutrients to the tissue, accelerating metabolic processes, promoting profound muscle relaxation, and immediately improving the range of motion while alleviating pain caused by muscle tension.
OmniLase®: Precision, Efficacy, and Patient Comfort
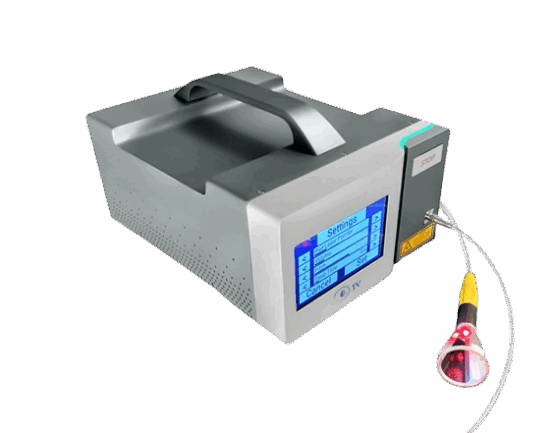
The Eclipse® – 980 and Eclipse® – IV from OmniLase® are state-of-the-art therapeutic laser systems designed to meet the rigorous demands of professional clinical environments. Our commitment to innovation ensures:
- Unmatched Uniformity of Illumination: Our systems deliver consistent energy across the treated area, crucial for predictable and effective outcomes.
- High Efficacy of Procedures: Precision engineering translates to superior therapeutic results.
- Ultimate Comfort for Patients: Gentle and effective treatment minimizes discomfort, ensuring a positive experience for every patient.
Equip your practice with OmniLase® and redefine the standard of care for your patients.
Recommended products